
Karli’s Reflux Journey – Awareness Week 2022
5 years ago; I found out I was pregnant. My 3rd pregnancy, amidst a journey of pregnancy loss, infertility and other such issues. It was Mother’s Day 2017. Back then, things like reflux, laryngomalacia, food aversions, postnatal depression, all were things I’d had little to no experience with, they weren’t even anywhere NEAR my radar of possibilities. I couldn’t have even TOLD you what laryngomalacia was, or what postnatal depression even felt like. I’d heard of “spilly babies” and “happy chuckers” – and I knew that people with breathing difficulties got pneumonia when they get colds. But that was the extent of my knowledge. Fast forward to Jan 2018. My little Emelia-Michelle was born in the late hours of the evening. She was induced a week early, and born after a very quick labour.
She would vomit frequently at the birth centre, and I was often told that this was fairly normal for babies who are induced, and induced early. So didn’t think a lot of it. I remember her first night so clearly. Everyone had told me about this big “after birth sleep” babies have. My little Emelia screamed. And screamed. She was as stiff as a board, and screamed. Nonstop. I had my friend staying with me at the birth centre; and we took turns with her all through the night. Eventually we buzzed for help. How an earth do we stop the baby screaming?? What is wrong with her? Neither of us have ever seen a baby scream like this. Let alone a newborn. The midwife wrapped her… tight. And sung to her. She had no idea why she was so distressed. She managed to calm her, and we syringe fed her; as her latch was poor. She had a really gnarly tongue and lip tie. This got remedied at a couple of days old, but still. The issues continued. Another midwife who came in said she’s probably just in pain, after her delivery, it’s to be expected. So as soon as we left the birth centre; we took her to a chiropractor. Who we visited every week for the next several weeks. No one knew why my baby was like this.
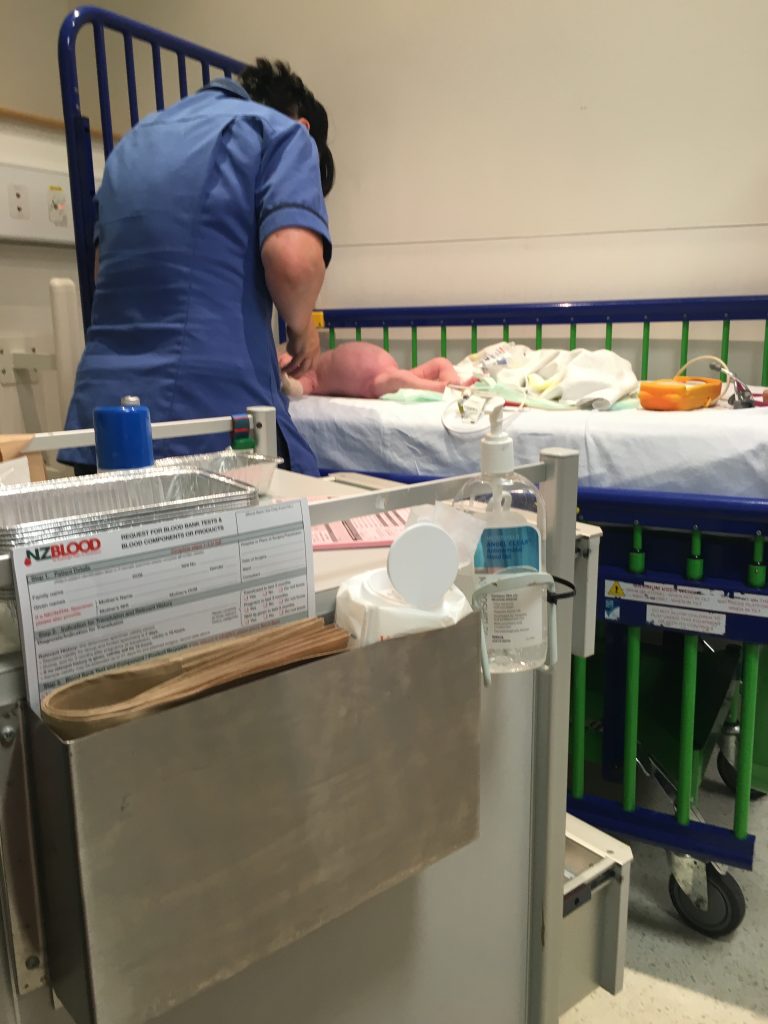
This was the start of our “reflux journey.” Emelia had a good 2 weeks of growth. Then it stopped. She ended up in the emergency department of Waikato Hospital at 14 days old vomiting fluorescent yellow liquid. Her stomach was extremely distended, and she was still so miserable. Surgeons came by, doctors left right and center. They scrambled to get IV lines in, and vials of her blood were laid out on a medical trolley with all sorts of different labels. Hirshprungs disease got thrown around, Pyloric stenosis. Gastroenteritis. Bowel intussusception. Basically everything under the sun. EXCEPT reflux. Fast forward another 3-4 weeks. And Emelia-Michelle is now 6 weeks old. She has literally screamed every minute of her life, only sleeping out of pure exhaustion. My midwife and I are stuck. I am feeding her breastmilk, and goats milk formula. We tried gaviscon. We tried infacol. We tried Weleda colic powder. With falling weight, poos filled with blood, and no idea why, we get back up involved; and see a pediatrician. Who diagnoses Emelia with a possible cow milk protein allergy.
I’m given a prescription for an allergy friendly formula to try, and instructed to remove dairy from my diet if I want to continue breastfeeding. I feel a relief. Not that there is something wrong with my baby. But that there is a reason she is screaming so much. She doesn’t just hate me. But the formula has her projectile vomiting, worse than ever. She hasn’t pooed in several days. She’s lost another 50 grams. So my midwife rings the pediatrician again. And we get a prescription for an Amino Acid based formula. I now have to cut soy out as well.
Emelia’s first year of life is mostly a blur. There was a lot of crying, from us both. You couldn’t hug Emelia. Family couldn’t even hold her. Everyone just assumes newborn babies like to cuddle, and sleep. But not this one. People told me – it was because I’m a stressed out first time mother. I was made to feel like the majority of our experiences were in my head. Yet she had an ear infection every month of her life, from about 3 months old. She had tonsillitis at 4 months old, and then battled that every month to 2 months. Her first case of pneumonia at 6 months old, which also became a reoccurring thing. She was vomiting blood frequently and regularly. Due to her severely burnt oesophagus. She couldn’t eat or drink without choking. She stopped breathing several times, and would EASILY starve herself upwards of 2-3 weeks due to oral aversion. I resigned from my job, because Emelia was just always unwell. I don’t understand how this looked like “in my head” when my little baby was failing to thrive. She was so unwell, and looking back – I feel so sad for her. That she had to suffer for so long. Knowing now, what I know.
On one of our many trips to ED at the hospital, at about 6 months old. We bumped into the pediatrician who had seen Emelia as a newborn. She is surprised we are still battling. She agrees to see us in her clinic in the coming weeks. And she diagnosis Emelia with severe reflux, severe CMPA and a severe soy protein allergy. She also can’t tolerate any fruit varieties either. Finally, finally. Emelia is put on medication – and we start to see small improvements. I finally felt like I had someone on my team.
At 9 months old Emelia is put on the wait list for grommet surgery. She has laryngomalacia. I’m diagnosed with post-natal depression. Emelia is on more medication than I’ve had in my entire life. And life, is really just at absolute rock bottom. My baby hates everyone and everything, I can’t bond with her, we are really just creeping along – surviving.
At about a year old, she gets her grommets, her adenoids are reduced. And the ENT and pediatric team tell me this little girl has very extensive damage due to the severity of her reflux. We slowly add to our medical teams as Emelia gets older and progresses through different stages of toddlerhood. Dieticians and SLT work together to manage Emelia’s choking, aspiration and pneumonia episodes, while keeping her nutrition content adequate due to her food aversions.
At 2 years, Emelia gets her second set of grommets. She has her now basically rotten tonsils removed. Her adenoids reduced – a second time. Her nasal passages cauterized to help her airflow and reduce congestion and constant blood noses she has been getting. She gets referred to rheumatology as her chronic infections have affected her immune system now causing sudden and spontaneous high fevers. There are more foods she CAN’T eat, than foods she is allowed.
3 years. Emelia is still on reflux medication, and still gets aspiration pneumonia – but she is finally turning a corner. Putting on weight. GROWING. Eating. Sleeping. We tried a medication wean, which resulted in a gnarly double ear infection, and chest infection – due to the milk rising through her airways and Eustachian tubes as she sleeps. But otherwise, she’s starting to function like a perfectly normal, healthy kid. She even finally cuddles people now. No longer in so much pain that even a simple cuddle is unbearable. Throughout this year I had started to consider transferring my final embryo. I had a discussion with doctors – is what Emelia has gone through; reoccurring?? And they assure me; no. It’s really – just crappy luck. My Dad is sick; dying. Fighting a cancer battle. So I decide to transfer this embryo; and hope for the best. I pray that he is able to stick around and meet this little baby. March 2021 I found out I was expecting again. I’m both ecstatic, but nervous.
Emelia-Michelle is SO excited to be a big sister; and of course we are eager to find out whether the baby is a girl baby or a boy baby. Emelia wants a baby brother called “Harry.” Yet in true style; at my 19-week scan. My littlest baby is suspected to have a wee hole in her heart. And a cleft lip, and/or palate. Seriously. WHY? I ask myself. I was so sure that after Emelia; I would be blessed with an easy child. But apparently not. We follow up with fetal med, and the heart issue has either resolved, or was never there. But the cleft lip and palate most definitely is there. Here we go again. As time goes, and I prepare for her life with a cleft – I hear; that a lot of cleft babies also have a bit of reflux. The dreaded R word…
Evie-Paul was born November 2021. 11/11. A lucky birthday some would say. My Dad didn’t make it to meet her. It was an emotional time for me, and little Emelia. But we embraced this wee girl that had finally joint us earth side. As soon as she was born; I felt instant connection to her. Emelia slotted into big sister life. And we were on cloud 9. Due to her cleft, we immediately had medical teams involved. Paeds, SLT, Cleft Coordinator. But really, she seemed “ok” – she couldn’t bottle feed, and she was a little unsettled. But nothing major. We had a fairly low key first week. But then her jaundice started to wear off, she started to wake up a little more. Crying episodes more and more frequent and her voice getting pretty hoarse and croaky. At 4 weeks old; We suspected reflux. Evie is admitted to hospital – she hasn’t drunk anything in several hours; she hasn’t pooed in about 10 days; she won’t stop screaming. They decide due to her feeding issues, and the severity of some gnarly blisters in her mouth – that we are best to insert an NG feeding tube. And they diagnose her with “Silent reflux.” A little different to Emelia’s as Evie doesn’t power chuck, in fact, she barely even spills.
Like Emelia; this worked. Until it didn’t. And at 7/8 weeks, our dietician suggests maybe a hint of CMPA coming out. So I start to eliminate dairy, and we try her on an allergy formula. However, like her big sister – the allergy formula made the reflux really flare up, and she was inconsolable. We went to stay in Waikato Hospital’s Mothercraft Unit, and did manage an NG tube wean. This was both hard, and therapeutic. I just felt stuck. We didn’t really achieve a lot in MCU this time. She still isn’t sleeping; the pediatrician accepts she has reflux – but is hesitant to increase medication at this point. We try the Amino Acid formulas that worked for Emelia; however, they just cause her reflux to worsen. She is turning blue during her choking/reflux episodes now. And I am too scared to even take her 5 minutes up the road in the car after a bottle. I am managing to pump breastmilk for her; but with post-natal depression rearing its head; I am also starting to resent ‘having’ to pump. I start to feel no easy out. I’m dairy free, soy free (precautionary) and also become egg free too after noticing differences when eating eggs.
Post Mothercraft; every day gets worse and worse. So our GP agrees to add different medications to the mix – and our homecare nurse liases with our pediatrician who agrees and signs off on this decision. She is the same one I had with Emelia. She knows us. And knows our history. So she isn’t surprised Evie is following in Emelia’s footsteps. The only difference is this time; Evie hasn’t had to suffer the same way Emelia had, there is suffering, but there is also treating, and working alongside medical teams. They KNOW it’s not in my head. In fact, several medication professionals now ask me – if I come from a medical trained background. Due to my knowledge, terminology, and the things I ask and point out. No, other than a first aid cert; I’m not medically “trained” at all. Not technically anyway. We are very much still in limbo with little Evie girl. She is 6 months old now; has had stage 1 (of many) of her cleft repair, her weight has gone from the 75th percentile, down to the 0.3rd. She is failing to grow and thrive. Worse than Emelia ever did. She is also diagnosed with a severe dairy allergy; but luckily seems to tolerate soy. However; she DOES have an IGE allergy to egg – and this scares me more than anything I’ve been through. As IGE allergies can be, and often are life threatening. Evie has terrible oral aversion; and almost every bottle she’s ever consumed has been a fight. Yet the NG holding her sphincter open wasn’t tolerated either. She doesn’t respond as well to medication very well; and we literally have to increase it every 3-4 weeks. We are now at a point of not being able to increase it anymore, or add any more options. We’ve used everything. We can’t get weight on Evie. She has oral aversion. Yet due to her cleft repair; we also now no longer have an NG as a fall back option. I really, honestly – don’t know what next.
I remember way back in the midst of Emelia’s battle. At rock bottom. I honestly was about to loose it at the next person who told me – she will outgrow it. Because truthfully I was adamant this was going to be life with her; forever. We’d never bond. She’d never thrive. I’d never have more kids. This was me. Done. Someone, in fact I can’t even remember who – referred me to “Crying over spilt milk.” I remember going on the website; and it just was so overwhelming. I didn’t want to accept help. I felt like I had to do everything on my own. Remember, it was all in my head? What good would seeking help do?? But a good friend of mine pushed me too it. She pushed me to treat the PND, and pushed me to seek support for Emelia’s reflux management. So I did. And suddenly; I wasn’t alone. There were other babies out there, Just like my own. Other Mum’s feeling; just like I was. The support from others in my exact position has far outweighed any advice ever given. The medical professionals treat the medical side. But having a support network; adding to MY bucket of people, MY village. Helps ME fight the reflux fight. And this is why, we are here now. Writing this post. Because while someone’s reflux battle could seem worse than your own, or it could even seem minor, I’ve come to learn – Reflux is reflux. It’s not easy, but it is all our own journey; and it is hard. But it doesn’t have to be scary, it doesn’t have to be lonely, it doesn’t have to be isolating. There is support out here, there is a village to help fight and get through it.
Across both girls we’ve used chiropractors, osteopaths, homeopaths and acupuncture. I’ve bought more natural remedies for reflux/colic/constipation than I can even count. I’ve administered omeprazole, ranitidine (now recalled/no longer available), gaviscon, famotidine, domperidone, ondansetron and buscopan between the girls. I’ve breastfed, syringe fed, cup fed, bottle fed, and tube fed. We’ve used puree baby food, and done baby led weaning. We’ve trialed regular cow milk formula, goat’s formula, lactose free formula, hydrolyzed formulas, and amino acid based formulas. Evie is currently managing soy formula. There are honestly; SO many options out there. The trick is finding the right treatment plan. If something doesn’t work, ask to try something else. If that doesn’t work. Change again. If the doctor won’t listen, find a doctor who will. Take photos, take videos, write everything down. If the fight is too hard alone; find someone who can do it for you.
I wish we hadn’t gone through what we went through. I know everyone says it makes you stronger, and to be proud of how we got through – but I’m not at that stage yet. Truthfully; it sucks. There is nothing worse than seeing your baby in pain, day in, and day out. Not being able to do a thing about it. Feeling like everyone thinks you’re making it up. Literally fighting medical professionals to understand. Crying in ED – because you just don’t know what to do anymore. But the biggest difference between then and now is. I SEE what Emelia has been through; I know now that she DID outgrow the worst of it. Yes, it took time, yes there was significant medical intervention. But she is doing well, she’s thriving, she’s well advanced for her age, she’s grown – and man, is she tall! She likely; will forever have issues. The damage to her lungs, and gut – could last forever. But what she lives with now; is nothing compared to her 3 years ago. It means I can now look at Evie; and I can tell myself she too will get to that point. I’m a lot more at peace about the journey. I still battle PND myself. PTSD. I live with anxiety daily. The lot. Life is not easy; in the slightest. But I can tell myself; I no longer have to get through a day at a time. If all I can get through in a moment, is 1 minute at a time – then so be it. Things might not be ok right now, but that IS ok. They will be ok one day. And if that is too much to manage, and that seems too far away – that is ok too.
I’m a lot more at peace about the journey.







© Karli Parsons and Crying Over Spilt Milk Gastric Reflux Support Network New Zealand May 2022.
You can contact the postnatal distress centre here http://www.postnataldistress.co.nz/
or visit https://pada.nz/
Or the depression helpline on 0800 111 757 Or free call or txt 1737 to talk
One of the risk factors for post-natal depression, is ongoing stress. A baby who spills a lot, vomits, screams or is otherwise unwell is an ongoing stress and shouldn’t be underestimated.
Perinatal Anxiety and Depression Aotearoa say this on their website “Parents who get the support and help that they need with parenting are more relaxed and better able to look after their children. If the mother or father is mentally unwell, extra support is essential to help with their recovery, and we encourage anyone to seek advice from a GP, Midwife, or Plunket nurse in the first instance.” https://pada.nz/national-helplines/– Jenny and Roslyn
These stories are our members’ personal experiences and opinions, and they are part of their healing process. Crying Over Spilt Milk Gastric Reflux Support Network New Zealand for Parents of Infants and Children Charitable Trust shall not be responsible or in any way liable for the continued accuracy of any information given, or for any errors, omissions or inaccuracies in these personal stories whether arising from negligence or otherwise, or for any consequences arising there from. Views expressed do not necessarily represent the views of the managers, coordinators or committee.





